This page contains usage statistics and a summary of the data submitted to the NDRLS nuclear medicine survey.
If you are conducting a publicly funded research project and would like to gain access to an anonymised version of the NDRLS MDCT dataset, please contact the NDRLS team.
Data sources and calculation methodology
The DRLs were derived from a survey, conducted in 2021/22, of nuclear medicine facilities. We asked participants to provide the prescribed activity for all procedures offered at their facility and to report every dose (from both radiopharmaceutical and CT sources) delivered within their facility over a two-week period.
Results from the 2021 nuclear medicine survey have been used to formulate the national DRLs for procedures on adult patients. In all cases, the DRLs have been based on the 75th percentile of the distribution of Facility Reference Levels (FRLs), where the FRLs are doses/activities indicative of common practice on a particular scanner at a particular facility.
How FRLs were defined varied for different modalities. For general nuclear medicine, the prescribed activity was generally used. A similar approach was used for PET, however facilities that based prescribed activity on patient weight (or a similar characteristic) were treated separately to those that delivered the same activity to all patients. For the CT component of SPECT/CT and PET/CT, an FRL was assigned to each scanner that conducted a particular scan type, with the value of the FRL being the median dose delivered to the patients included in the survey.
The metric chosen to define the DRLs was the 75th percentile of the FRL distribution, keeping the nuclear medicine DRLs consistent with the CT DRLs already published by ARPANSA. In addition to the DRL, the 50th and 25th percentiles of the distributions were also calculated.
Community participation
ARPANSA engaged Services Australia to send invitations to all facilities listed on the Location specific practice number register that are accredited to offer nuclear medicine services. Services Australia reportedly sent approximately 300 invitations. Table 1 contains the number of facilities that engaged with the survey and Table 2 shows the number of facilities and scans included in the final dataset.
Table 1: The number of facilities that engaged with the survey. Note that a single facility could register for both the NM and PET components of the survey, hence the Total column isn’t simply the sum of the other two columns.
| NM facilities | PET facilities | Total | |
|---|---|---|---|
| Registered | 108 | 59 | 127 |
| Submitted survey | 92 | 45 | 107 |
| Included in analysis | 86 | 44 | 99 |
Table 2: The data reported by facilities from which data was used when determining DRLs
| Number of facilities | Number of scans | |
|---|---|---|
| General nuclear medicine | 86 | 6201 |
| NMCT | 82 | 3784 |
| PET | 44 | 4322 |
| PET/CT | 44 | 4258 |
Submitted data
Summaries of the number of surveys submitted and the number of scans reported are presented in tables 3 to 7. Also included in the tables are the 25th, 50th and 75th percentiles of the FRL distributions and, where appropriate, the most common activity reported. The FRL distribution for all protocols can be accessed by clicking the entries in the DRL tables on the Current NM DRLs page.
Table 3: The general nuclear medicine protocols reported by NDRLS survey participants. Only the protocols that were used to develop the DRLs are shown.
| Percentiles (MBq) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Category | Scan | Pharmaceuticals | No. FRLs | No. scans | 25th | 50th | 75th | Most common activity (MBq) | |
Cardiovascular |
Gated blood pool scan | Pertechnetate, RBCs | 72 | 180 | 878 | 953 | 1000 | 1000 | |
| MPI 1-day: | 1st phase (rest) | Tetrofosmin, MIBI | 52 | 411 | 300 | 305 | 350 | 300 | |
| 2nd phase (stress) | Tetrofosmin, MIBI | 51 | 371 | 900 | 1000 | 1150 | 1000 | ||
| MPI 2-day | 1st phase | Tetrofosmin, MIBI | 41 | 163 | 350 | 500 | 600 | 600 | |
| 2nd phase | Tetrofosmin, MIBI | 41 | 163 | 350 | 500 | 600 | 600 | ||
Endocrine |
Thyroid | Pertechnetate | 84 | 199 | 200 | 200 | 200 | 200 | |
| Parathyroid | Without subtraction | MIBI | 31 | 43 | 750 | 800 | 800 | 800 | |
| With subtraction | MIBI | 49 | 71 | 750 | 800 | 900 | 800 | ||
| Thyroid subtraction | Pertechnetate | 50 | 58 | 40 | 60 | 220 | 40 | ||
Gastrointestinal |
Gastric emptying (solid phase) | Colloid, DTPA | 81 | 125 | 40 | 40 | 40 | 40 | |
| Colonic transit | 67Ga Citrate | 75 | 27 | 10 | 20 | 20 | 20 | ||
Hepatobiliary |
Hepatobiliary | HIDA, DISIDA, Mebrofenin | 81 | 67 | 200 | 250 | 300 | 200 | |
Infection |
Infection | 67Ga Citrate | 70 | 25 | 200 | 200 | 220 | 200 | |
Lymphatic |
Sentinel node (breast)†: | Same day surgery | Colloid | 75 | 229 | 20 | 40 | 40 | 40 |
| Delayed | Colloid | 32 | 59 | 42 | 80 | 80 | 80 | ||
| Sentinel node (melanoma)† | Colloid | 65 | 49 | 20 | 40 | 52 | 40 | ||
Nervous system |
Brain | ECD, HMPAO | 66 | 170 | 740 | 750 | 800 | 750 | |
Pulmonary |
Lung perfusion | MAA | 82 | 455 | 200 | 200 | 220 | 200 | |
Skeletal |
Bone scan | MDP, HDP | 85 | 1962 | 800 | 825 | 900 | 800 | |
|
† Quoted activities are the total delivered, not per injection. Table 4: The CT scans reportedly conducted as part of a SPECT/CT scan. Note that brain scans are not included here as the brain NMCT DRL was not updated for the 2023 DRLs. Only the protocols that were used to develop the DRLs are shown.
Table 5: The variable prescribed activity PET protocols reported by NDRLS survey participants. Only the protocols that were used to develop the DRLs are shown.
Table 6: The fixed prescribed activity PET protocols reported by NDRLS survey participants. Only the protocols that were used to develop the DRLs are shown.
Table 7: The CT scans reportedly conducted as part of a PET/CT scan. Note that brain scans are not included here as the brain PETCT DRL was not updated for the 2023 DRLs. Only the protocols that were used to develop the DRLs are shown.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
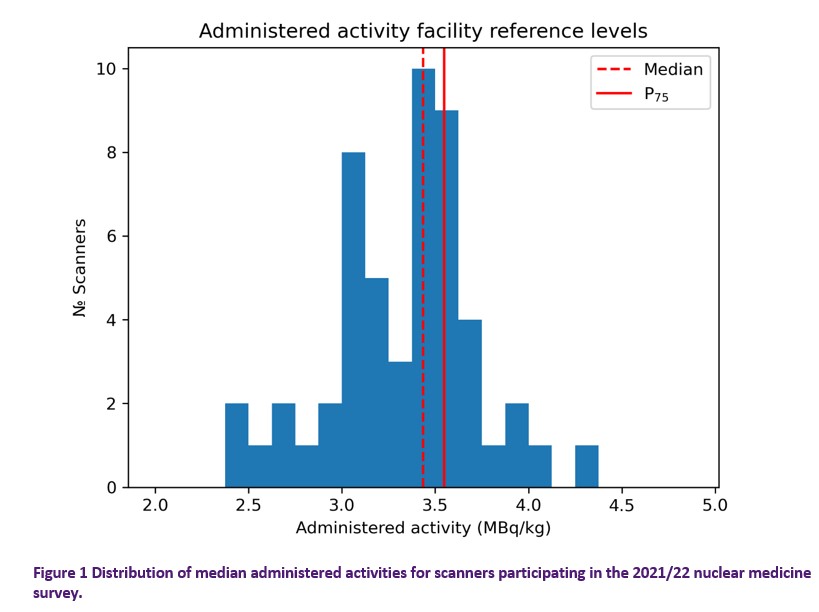
Note that the 75th percentile of this FRL distribution is slightly higher than the DRL (3.55 MBq/kg compared to 3.5 MBq/kg). This is fairly typical of the data submitted to the survey for all procedure types, facilities tend to administer slightly higher doses than they prescribe. Table 8 provides additional summary statistics of the FRL distribution.
Table 8 Summary statistics from the scanner level FRL distribution shown in Figure 1. With the exception of the number of scanners, all values are expressed in terms of MBq/kg.
|
Number of scanners |
52 |
|
Mean |
3.33 |
|
Standard deviation |
0.40 |
|
Minimum |
2.39 |
|
25th percentile |
3.03 |
|
Median |
3.44 |
|
75th percentile |
3.55 |
|
Maximum |
4.38 |
Time Activity Product
Of the 3322 scans reported, 2972 (from 49 scanners) provided the make and model of the scanner used and an indication of the scan time per bed position. Having the scan time per bed allows for the calculation of the time activity product (TAP), which theoretically provides an indication of the achievable quality of a scan.
All else being equal, a larger TAP means more counts in an image and a higher quality image. In practice, differences in bed field-of-view, bed-position overlap, detector efficiency, reconstruction techniques and patient characteristics mean that TAP isn’t a direct comparator of quality, however it is worthy of consideration.
The TAP can be expressed in MBq.min/bed or, if the weight of the patient being imaged is considered, MBq.min/bed.kg (henceforth referred to as TAPw). The median TAPw values reported from scanners in ARPANSA’s nuclear medicine survey are shown in Figure 2. If you find that your dose is unusually high or low, it is worth comparing the TAPw used at your facility with the distribution displayed in Figure 2; it may provide an indication as to whether you are obtaining images with relatively high or low counts or if you simply use a different balance of dose and imaging time.
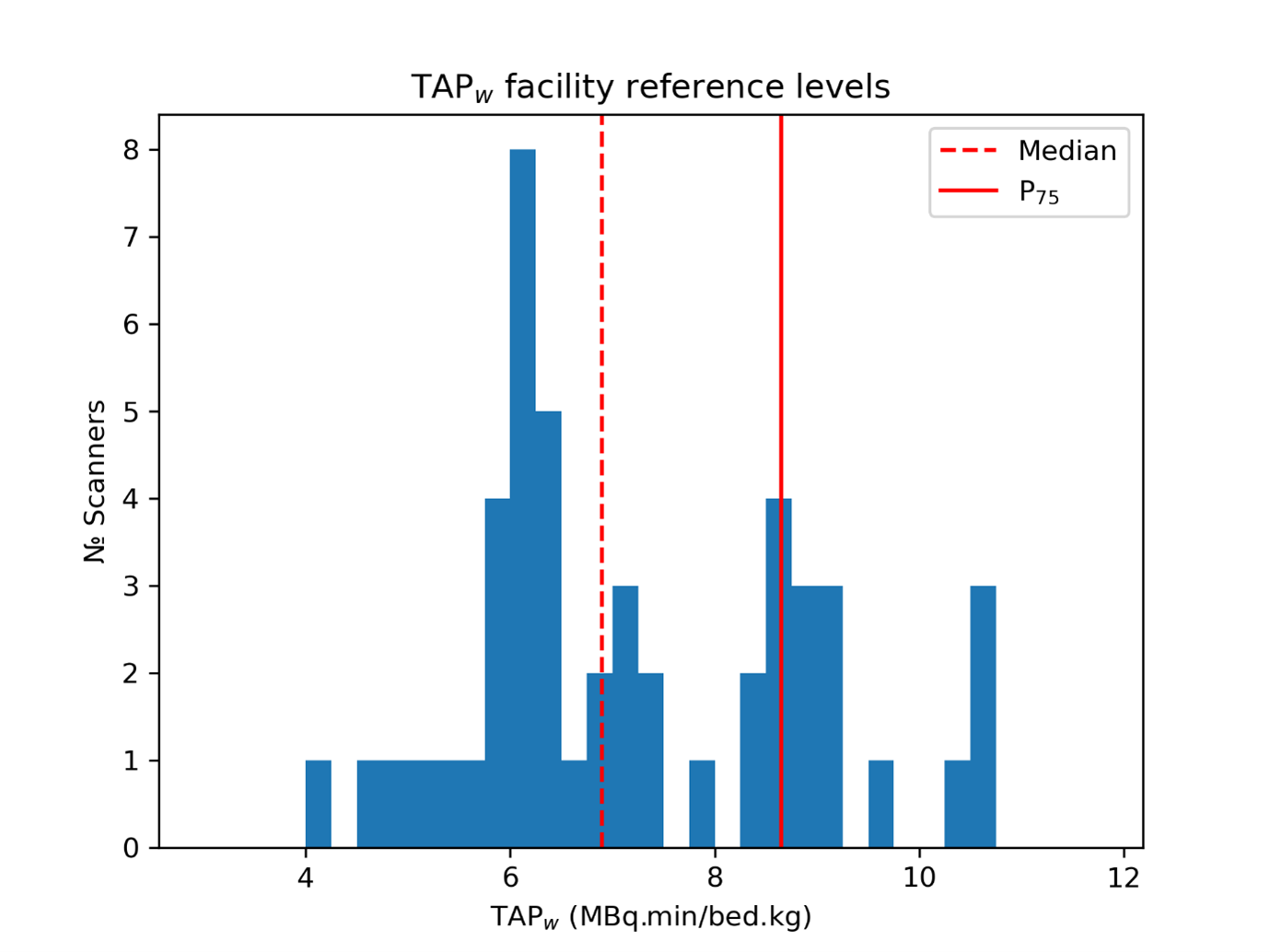
Figure 2 Histogram of the median weight dependent time activity products reported on each scanner.
TAPw is used by the European Association of Nuclear Medicine to set minimum recommended doses (links to a pdf), with a value of 7 MBq.min/bed.kg suggested as the minimum TAPw for PET whole body FDG scans. For comparison, the median TAPw shown in Figure 2 suggests that over half of the survey cohort routinely use a TAPw lower than the EANM recommended minimum.
Facility Type
Figure 3 and Table 9 summarise the median dose, time per bed, and TAPw reported to the nuclear medicine survey, classified by the funding model of the reporting facility. There were 3 facilities that identified themselves as being a private company in a public facility, for the purposes of this analysis these facilities have been reclassified as private.
Private facilities reported using lower doses and scanning for broadly similar time per bed as public facilities. This resulted in private facilities reporting lower TAPws.
Table 9 Summary statistics of the FRL distributions of administered dose and TAPw for the different facility types that participated in the nuclear medicine 2021/22 survey.
|
Administered dose (MBq/kg) |
TAPw (MBq.bed/min.kg) |
||||||
|
Scanners |
25% |
50% |
75% |
25% |
50% |
75% |
|
|
Private |
30 |
3.01 |
3.16 |
3.48 |
6.03 |
6.32 |
7.33 |
|
Public |
19 |
3.25 |
3.57 |
3.73 |
6.38 |
8.62 |
9.04 |
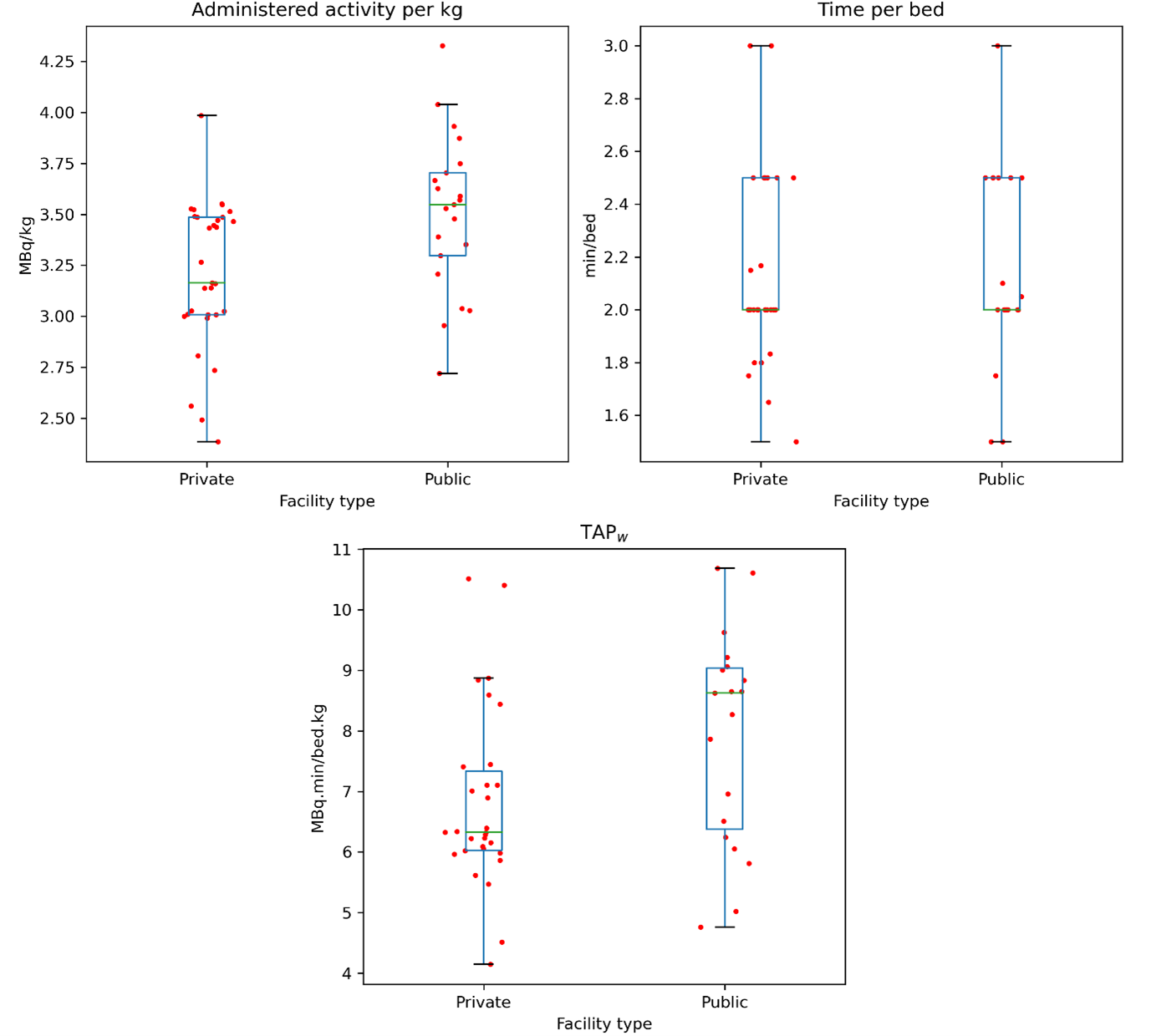
Figure 3 Boxplots of median dose and time metrics classified by facility funding type. Note that the overlayed scatter plots have had a “jitter” applied to make visualisation clearer, there is no underlying meaning to the relative x position
Detector type
In recent years, solid state photomultiplier technology has become available on clinical PET systems. Only six silicon photomultiplier (SiPM) scanners submitted data to the 2021/22 NDRLS nuclear medicine survey (including one that was a whole-body system) and only four of those scanners provided time data.
The doses administered to patients undergoing exams using the SiPM scanners was lower, however there are too few such scanners to draw any broad conclusions about their relative performance. Furthermore, it is clear from Table 10 that the SiPM scanners do not have a strong influence on the overall distribution of dose and scan times.
Table 10 Summary statistics of the FRL distributions of administered dose and TAPw for SiPM based detectors compared to PMTs.
|
Administered dose (MBq/kg) |
|
TAPw (MBq.bed/min.kg) |
||||||
|
Scanners |
25% |
50% |
75% |
Scanners |
25% |
50% |
75% |
|
|
PMT |
46 |
3.031 |
3.468 |
3.551 |
45 |
6.158 |
6.958 |
8.7 |
|
SiPM |
6 |
2.967 |
3.177 |
3.38 |
4 |
4.958 |
5.443 |
6.5 |
Most common scanners
Figure 4 and Table 11 summarise the distribution of administered activity and TAPwFRLs recorded using the three most common scanner models. The information is presented to allow users of the listed scanners to compare their administered activities and TAPws with their most similar counterparts, it is not to compare the merits of the three included scanners.
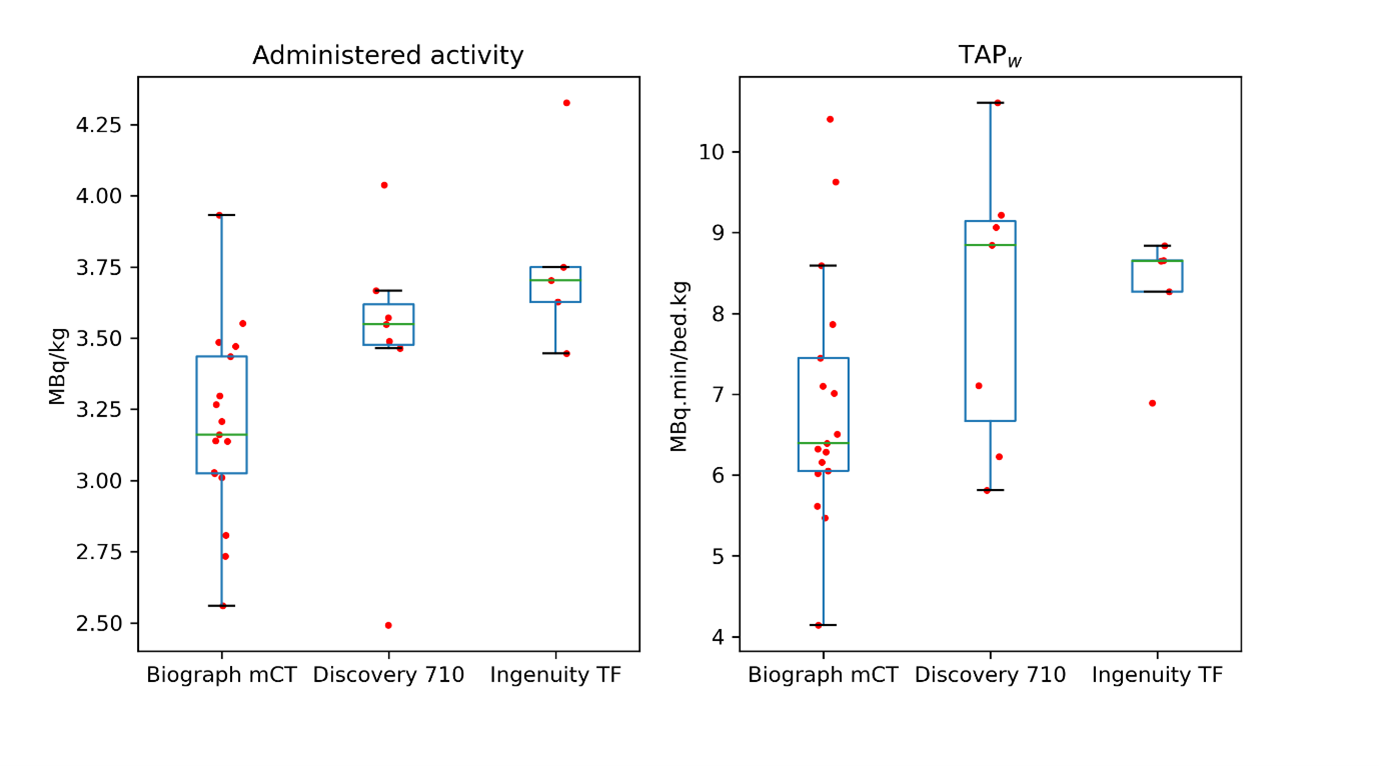
Table 11 Summary statistics of the FRL distributions of administered dose and TAPw for the three most common scanner models within the nuclear medicine 2021/22 survey cohort.
|
Activity (MBq/kg) |
TAPw (MBq.bed/min.kg) |
|||||||
|
Make |
Model |
Scanners |
25% |
50% |
75% |
25% |
50% |
75% |
|
Siemens |
Biograph mCT |
18 |
3.03 |
3.18 |
3.46 |
6.029 |
6.357 |
7.362 |
|
GE |
Discovery 710 |
7 |
3.48 |
3.55 |
3.62 |
6.668 |
8.843 |
9.14 |
|
Philips |
Ingenuity TF |
5 |
3.63 |
3.70 |
3.75 |
8.268 |
8.65 |
8.653 |